Table of contents
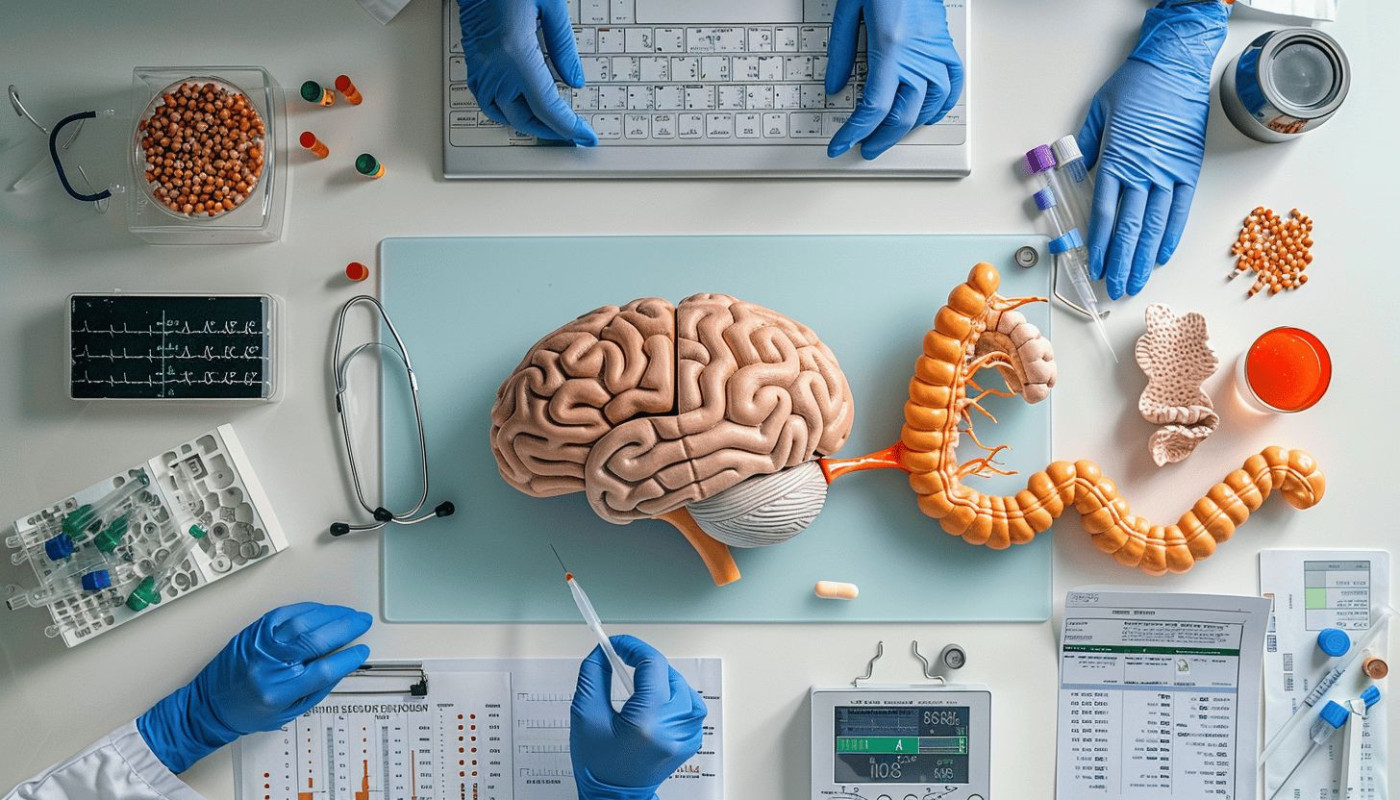
The intricate dance between gut health and mental well-being is an enthralling topic that is garnering significant attention in both the scientific community and the public sphere. This connection, often referred to as the "gut-brain axis," suggests that the state of our digestive system can profoundly influence our mood, stress levels, and overall psychological health. As we peel back the layers of this complex relationship, the potential for improved mental wellness through gut health becomes evident. Read on to discover how nurturing your gut could be the key to unlocking a happier, more balanced state of mind.
The Gut-Brain Connection
The biological basis for the gut-brain connection, often referred to as the gut-brain axis, lies in the sophisticated dialogue between our central nervous system (CNS) and the enteric nervous system (ENS). This complex network involves a bidirectional communication system, where not only does the brain send signals to the gut, but the gut conversely relays messages back to the brain. A key player in this interaction is the vagus nerve, one of the longest cranial nerves in the body, which acts as a critical information highway, transmitting signals between the gut and the brain.
Neurotransmitters, chemicals responsible for transmitting messages from nerve cells to target cells, are pivotal to the functioning of this axis. Interestingly, a large proportion of these neurotransmitters, including serotonin, which is central to mood regulation, are produced in the gastrointestinal tract. The gut microbiota, the trillions of microorganisms residing in our intestinal system, also play a significant role. These microbial populations influence the production of neurotransmitters and can directly affect the signaling of the gut-brain axis.
Emerging research has spotlighted a particular category of microbes known as "psychobiotics," which have the potential to produce and deliver neuroactive substances, such as gamma-aminobutyric acid (GABA) and serotonin, that can positively impact mental health. The study of psychobiotics is a field that neurogastroenterologists and researchers are delving into, with the aim to better understand the intricate connections between gut health and mental well-being. This research suggests that by modulating our microbiome, we may be able to enhance our mood and cognitive functions, paving the way for innovative treatments for mental health disorders.
Microbiome and Mood
The intricate link between the gut microbiome and mental well-being is gaining increasing attention in the field of psychosomatic medicine. A delicate balance of bacteria within the gut can significantly impact mood and overall mental health. An array of studies has elucidated a correlation between dysbiosis, an imbalance in gut bacteria, and mental health conditions such as depression and anxiety. These associations arise from the complex communication network between the gut and the brain, known as the gut-brain axis. Probiotics, the beneficial bacteria found in certain foods and supplements, have been identified as a potential strategy for modifying gut flora. By doing so, they may offer promising avenues for improving mental well-being.
Research has revealed that individuals with healthy and diverse gut microbiomes tend to have lower risks of developing mood disorders. Conversely, profiles of gut microbiota that deviate from the norm have been observed more frequently in those suffering from depression and anxiety. This suggests that the presence or absence of specific bacterial strains in the gut may play a role in mental health outcomes. Addressing dysbiosis through targeted probiotics might help restore a healthy balance within the gut microbiome, potentially leading to mood stabilization and enhanced emotional resilience.
The potential benefits of probiotics include not only the restoration of a healthy gut ecosystem but also the production of neurotransmitters like serotonin, which plays a pivotal role in mood regulation. Furthermore, the anti-inflammatory properties of certain probiotic strains could mitigate the inflammation often associated with mental health disorders. While the research is still burgeoning, the current findings offer a compelling case for considering gut microbiome interventions as part of a holistic approach to mental well-being.
Diet and Mental Health
The interplay between nutrition and well-being is a vast and intricate field, particularly when considering the effects of a gut-healthy diet on mental health. There is increasing evidence that the foods we consume have a profound impact on our gut microbiome, which in turn, influences our mental state. A diet rich in prebiotics, such as those found in fiber-rich foods, is pivotal for nourishing the beneficial bacteria in the gut. These prebiotic fibers are not digested by the human body but are instead utilized by the gut microbiota, encouraging their growth and activity.
Moreover, the inclusion of fermented foods in one's diet introduces beneficial bacteria and can help to enhance the diversity and resilience of the gut microbiome. A diverse microbiome is linked to better overall health, including improved mental health outcomes. Dietary choices that promote a balanced and diverse gut flora are therefore seen as a supportive approach to managing mood disorders.
Furthermore, an anti-inflammatory diet is another dietary approach that has been shown to have potential benefits for mental health. Chronic inflammation is often associated with the development of mood disorders, and a diet that can help reduce inflammation may also contribute to better mental health. By focusing on foods that reduce inflammation, individuals may notice an improvement in mood and cognitive function. It is worth noting that a specialist in the field, such as a dietitian or nutritionist with expertise in the gut-brain axis, would be an invaluable resource for those looking to enhance their mental well-being through dietary adjustments. Their guidance can help tailor a gut-healthy diet that considers individual nutritional needs while aiming to improve both gastrointestinal and mental health.
Stress, Anxiety, and the Gut
The intricate connection between stress and gut health is a topic of increasing study and concern among mental health professionals and stress researchers. Exposure to chronic stress has been shown to significantly impact gastrointestinal health, often leading to a variety of digestive problems. This can manifest as an upset stomach, irritable bowel syndrome, or even increased gut permeability, which is a condition more commonly referred to as 'leaky gut.' The bidirectional nature of this relationship means that just as stress can wreak havoc on the gut, the state of one's gut health can also influence stress responses and anxiety levels.
Managing stress is vital for maintaining a healthy gut. Techniques such as mindfulness practices can help individuals become more aware of their stressors and bodily responses, thereby providing a mechanism for better stress management. Regular physical exercise is not only good for the body but also for the gut, as it helps reduce the symptoms associated with stress and anxiety. Ensuring adequate sleep is yet another supportive strategy, aiding in both digestive and mental well-being. By addressing chronic stress through these various methods, one can help safeguard their gastrointestinal health and, in turn, potentially alleviate some of the psychological distress associated with anxiety.
Future Directions in Gut-Brain Research
The burgeoning field of gut-brain research continues to illuminate the complex interactions between our digestive systems and mental well-being. As we delve deeper into the intricacies of this connection, the horizon promises innovative mental health treatments stemming from an improved understanding of gut health. Clinical studies are pivotal in charting the course forward, with a particular focus on psychobiotic therapy—a frontier that explores the use of beneficial bacteria to exert psychological effects. Given the nuanced nature of gut-brain mechanisms, there is a pressing necessity for comprehensive research to unravel the specific pathways through which the gut influences neural processes. Neuroinflammation, a term referring to inflammation within the nervous system, is one such area that could unlock new understanding of psychiatric disorders. As the scientific community delves into the gut-brain nexus, the potential to revolutionize the approach to mental health looms large, underscoring the imperative for sustained investigation and collaboration among experts in the field.
Similar articles

Genetic Predisposition: Master or Servant of our Health?

Unlocking the Secrets of Ageless Beauty

Mindful Movement: The Psychosomatic Impact of Exercise

De-stress and Rejuvenate with Natural Therapies